Since the early 1990s, in most of the countries globally, antiretroviral medicines have been prescribed for post-exposure prophylaxis (PEP) following occupational exposure to the human immunodeficiency virus (HIV). This practice has since been extended to non-occupational situations, such as cases of sexual assault.
Increasingly, however, both policy-makers and health care providers have been raising questions about certain aspects of the use of HIV PEP: in particular, about the indications for post-exposure prophylaxis, the most suitable antiretroviral medicines to use, and various issues relating to prescribing protocols and clinical management. Awareness of these areas of uncertainty has been further heightened by the expanding availability of antiretroviral therapy in more resource-constrained settings and has led to calls for clear operational guidance on providing PEP.
According to the World Health Organisation (WHO), the term post-exposure prophylaxis is generally understood to mean the medical response given to prevent the transmission of blood-borne pathogens following a potential exposure to HIV.
Additionally, in the context of HIV, post-exposure prophylaxis refers to the set of services that are provided to manage the specific aspects of exposure to HIV and to help prevent HIV infection in a person exposed to the risk of getting infected by HIV. Post-exposure prophylaxis aka PEP should be given within 72hours from the time of exposure.
Types of exposure include; occupational exposure whereby, a needle prick of an infected person or unknown status, blood or fluid splash into the eyes from an infected person. Non occupational exposure for-example involvement in road traffic accidents, in-case there is sharing of blood between people of unknown status; sexual that can be rape, defilement or intimate sex from an HIV positive person or unknown status; human bite from an HIV positive person or unknown status.
Incase of any of the above exposures or contacts, the victim is supposed to visit the nearest health facility before the 72 hours elapse; explain everything that happened to the health care personnel, who will then perform an HIV test. Incase results are positive, other procedures will be followed to initiate one on treatment. Always remember ” the earlier the better”, and incase it’s negative, one will be initiated on a prophylactic/preventive treatment (PEP) for HIV/AIDs. This is taken daily and at the same time for a period of 28days. After completion of this treatment, the exposed person waits for more two weeks to make it 6weeks and gets tested again. At 12 weeks, if the test result is negative, one can be declared HIV free.
We therefore encourage everyone in the community to always advise and report cases of rape, incest, and any-other cases that expose one to HIV to the nearby health facility, police and relevant entities for timely interventions. Remember, taking medication for 28days is better than taking it for a lifetime. Therefore, do not miss out this chance. The beauty about this is that, all these services are free in all government health facilities in Uganda.
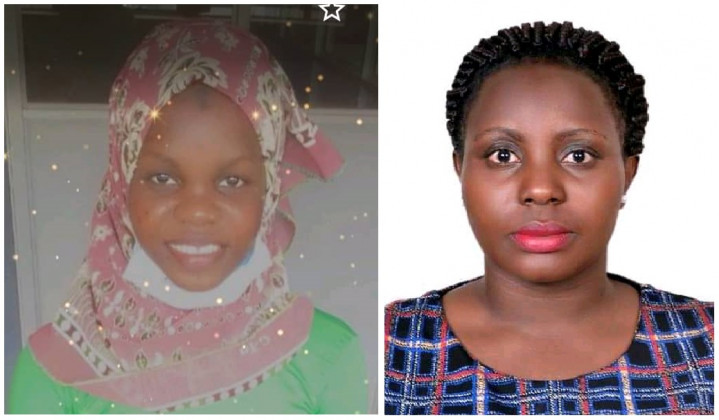
The authors are; Ms. Aisha Naiva, BScN Nurse and Nurse dispenser & Pharmacovigilance focal person at Kawolo General Hospital and
Ms. Lilian Nuwabaine, BScN Nurse & MSN-Midwife & Women’s’ Health Specialist working with Aga Khan University and is the HIHA Midwife of the year 2021
If you would like your article/opinion to be published on Uganda’s most authoritative news platform, send your submission on: [email protected]. You can also follow DailyExpress on WhatsApp and on Twitter (X) for realtime updates.