By Brian Nambale
As we commemorate World Meningitis Day every 5th of October every year, Uganda is also among the countries wrapped in the waist by the meningitis belt. The meningitis belt stretches across Africa from Senegal in West Africa to Ethiopia in the East where over 30,000 cases are reported each year according to the African Centre for Disease Control. Sub-Saharan Africa including Uganda has reported more cases in the past years.
Meningitis commonly called Mulalama in the local dialect is easily confused with Malaria, cold or any type of fever-causing illness including witchcraft or possible injury because, in its early times, the signs and symptoms are similar to all those.
Meningitis is a possibly fatal disease if not promptly recognized and treated. A multidisciplinary approach should be utilized to improve patient outcomes and deliver comprehensive care.
One of the reasons many people die is presenting to the hospital very late when the disease is very severe; associating it with witchcraft and refusal of a lifesaving procedure Lumbar puncture (taking off “water” from the back using a needle) which is so important in diagnosis & treatment of this disease.
What you need to know about Meningitis
The layers that cover the brain are called Meninges so meningitis is the inflammation (swelling) of these layers that protect of the brain and spinal cord.
Meningitis is usually caused by Bacterial & viruses, however, other forms of presentation include Neonatal meningitis, meningococcal disease and pneumococcal meningitis caused by Streptococcus pneumonia, fungal meningitis due to the low immune system especially in HIV/AIDS & Tuberculosis, Group B streptococcal meningitis, especially in babies.
These can be identified by good Clinical history, examination and laboratory check-ups.
Signs & symptoms of Meningitis
Meningitis is not always easy to recognize because it has signs similar to other diseases such as malaria. Meningitis can be recognized from the following signs;
- Fever
- Severe Headache
- Fast breathing / breathless
- Vomiting
- Very sleepy or unconscious
- Confusion
- Fits/convulsions
- Pale skin with cold hands and feet
- Stomach pain/diarrhea
- Aches & pains (severe limb or joint pains)
Common symptoms in young children are;
- Blank staring look
- Stiff neck
- Fear or dislike light
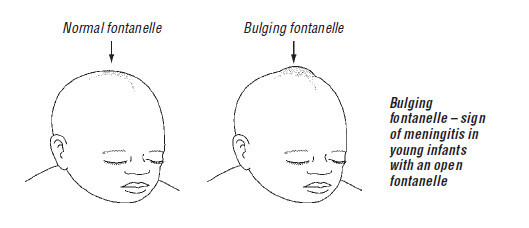
- Bulging or tense soft spot(fontanel locally called kawompo) on the heads of babies


How does one get Meningitis?
Most types of bacteria that cause meningitis are carried in the back of the nose and throat of some people. This is normal and many people carrying the bacteria will never get meningitis.
Sometimes, the bacteria invade the body via the back of the nose and throat and cause disease. The bacteria travel in the bloodstream to the lining around the brain and spinal cord and the infection makes this lining swell. The swelling presses on the brain and, if not treated quickly, can permanently damage the brain or kill the patient.
The bacteria that cause meningitis can be passed from person to person by breathing in droplets from the nose and throat of an infected person. Close and prolonged contact – such as kissing, or sneezing or coughing near others, or living in the same household as someone who is carrying the bacteria in their nose and throat – helps the bacteria spread more easily. Other risk factors include poor hygiene, smoking tobacco or exposure to cooking smoke, overcrowded settings (in schools, refugee camps or dancehalls or concerts / Bi’vulu) and missing routine recommended vaccinations.
Who is at risk?
Anyone of any age can get meningitis. Babies, young children, teenagers, elderly people and also people with weakened immune systems are most at risk.
How is Meningitis Treated?
Meningitis can kill within 24 hours, so fast referral and treatment is very important. It should always be viewed as a medical emergency and referral for treatment at a hospital or HCIV is necessary.
This will enable the health workers to provide the strong medicines required for its management and also to observe the patient.
Medicine used to treat meningitis cannot be bought from the pharmacy or given at HCII or HCIII, it can only be given at HCIV or hospital. This is why fast referral to the right place is very important.
How can you prevent Meningitis?
- The best way to prevent meningitis is to make sure all children are routinely immunized. The routine immunization schedule in Uganda includes vaccines against pneumococcal and Haemophilus influenzae type b (Hib) infections at 6, 10 & 14(Six, Ten & fourteen) weeks at childbirth. Immunization campaigns are sometimes carried out against some kinds of meningococcal bacteria (for example the meningitis immunization campaign carried out in northern Uganda in 2017, which was for meningococcal group A or MenA).
However, there are causes of meningitis that cannot be prevented with vaccines so it is also important to be aware of the signs and symptoms that should trigger referral. In Uganda
- Sometimes there are outbreaks of meningitis in an area and many people can be affected. To prevent the spread of disease, it is important to report cases to the health authorities quickly.
- Communities are advised to avoid gatherings or overcrowded places if there is an outbreak, the risk of contracting the disease is minimized.
- The public is encouraged not to neglect their health conditions and take regular yearly checkups. This prevents people from getting this disease, and diagnosis at the earliest if encountered
Appropriate hospital care and treatment are essential if the patient is to make a good recovery.
After recovery life-long after-effects normally appear such as;
- Loss of a limb or loss of ability to move easily without help from others or without using a tool like a wheelchair or artificial limb.
- Loss of hearing, learning difficulties, finding it hard to concentrate or communicate, or loss of sight (less common).
- Headaches, fatigues, behavior changes, convulsions/fits.
- Late complications of meningococcal meningitis include chronic pain, skin scarring, and neurologic impairment. Other common complications include hearing impairment, visual impairment(brain and nerve damage), and Fits/seizures. Hearing tests are recommended four weeks after hospital discharge. Post-traumatic stress disorder can also ensue; management may require psychiatric or psychological intervention
It should be noted that Physical and occupational rehabilitation is needed to minimize long-term complications and improve the quality of life in patients with meningitis.
Therefore, Know the signs and save lives; Don’t underestimate your consciousness act first and Defeating meningitis matters let’s do it together.
Key Facts to Know:
- Meningitis can affect anyone of any age
- Meningitis can kill if Medical action is not taken early
- Meningitis can cause long-term effects including learning disabilities in children among others.
- Viral and bacterial are the most common causes of Meningitis
- Early signs and symptoms can appear similar to flu and malaria
- Meningitis is a medical emergency presenting with severe sepsis syndrome (septicaemia).
About the Author: Brian Nambale (Hon.), is an Advisory Council Board Member (Africa) to the Confederation of Meningitis Organizations (CoMO) Part of the Meningitis Research Foundation (MRF);
If you would like your article/opinion to be published on Uganda’s most authoritative news platform, send your submission on: [email protected]. You can also follow DailyExpress on WhatsApp and on Twitter (X) for realtime updates.



